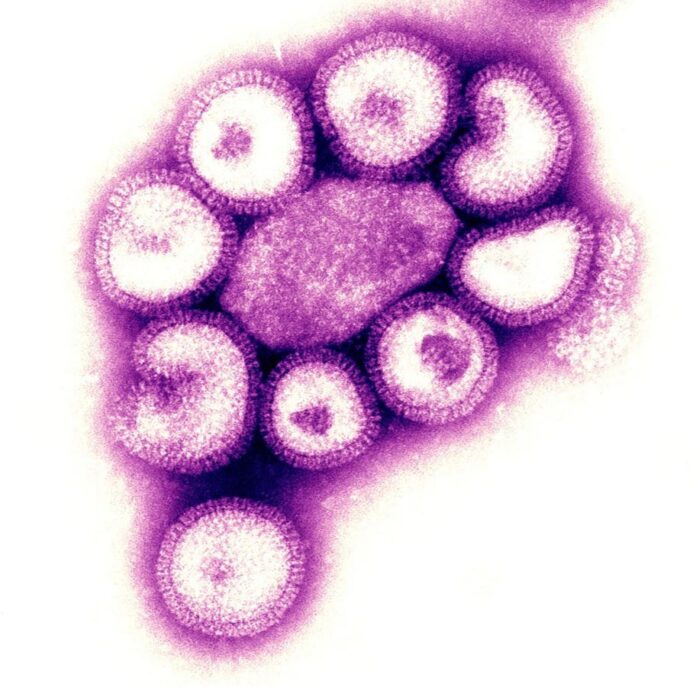
A more aggressive variant of the seasonal flu, specifically the Influenza H3N2 virus (subclade K), is gaining ground in the United States and across the northern hemisphere. This strain has already triggered an influenza epidemic in Japan and a surge in cases in the U.K., and while current flu activity in the U.S. remains relatively low, infections are climbing.
What Makes This Strain Different?
The H3N2 virus is known for causing more severe illness than some other flu types, and this new subclade K variant appears to amplify that trend. Symptoms mirror those of typical influenza – fever, cough, fatigue, muscle aches, and chills – but cases tend to be more intense, particularly in children and the elderly. Higher fevers are common, increasing the risk of complications like dehydration, breathing difficulties, and hospitalization. This isn’t a new phenomenon; H3N2 dominated the 2016-2017 flu season with similar effects.
Tracking Challenges and Data Gaps
One complicating factor is the limited data available on the spread of subclade K in the U.S. A recent 44-day government shutdown disrupted CDC tracking efforts, making it difficult to assess recent trends. The CDC’s latest FluView report does not specify circulating subclades, and it’s unclear if this detailed data will be released in the future. The variant was first identified in Europe in June and has spread rapidly since then, accumulating seven mutations.
Does the Flu Shot Offer Protection?
The current 2025-2026 flu vaccine is designed to protect against two Influenza A strains (H1N1 and H3N2) and one Influenza B strain. While the vaccine does target H3N2, it was formulated before subclade K emerged, meaning it’s not a perfect match.
However, vaccination remains critical. The goal isn’t necessarily to avoid infection entirely, but to reduce the severity of illness, lower hospitalization rates, and prevent fatalities. Data from the U.K. suggests the vaccine offers up to 75% protection for children and 40% for adults against subclade K when considering hospitalizations.
Getting vaccinated will still provide some level of protection against this variant, even if it’s not a perfect fit.
Staying informed and taking preventative measures – like getting vaccinated, practicing good hygiene, and staying home when sick – remains the best defense against this evolving threat.
The spread of this new variant underscores the constant need for surveillance and adaptation in influenza prevention efforts.